Quickstatus
Enthusiast
- Joined
- Oct 13, 2013
- Posts
- 17,606
That's a lot of atrial ectopics - almost even flutter. The 3rd sharp peak is an extra one that you may feel as an extra "beat"
That's a lot of atrial ectopics - almost even flutter. The 3rd sharp peak is an extra one that you may feel as an extra "beat"
Thankyou Sir!Don't hesitate to reach out by PM.
An ablation for non-sustained atrial or ventricular ectopics is an over-kill. I’ve never heard of anyone doing an ablation for premature atrial contractions because they often arise from multiple sites; you would just be chasing atrial ectopics and creating extensive scar—this is simply not done. On very rare occasions (last resort) you can have an ablation for premature ventricular contractions if they’re very frequent and highly symptomatic (>15% of total beats on Holter) or the PVCs are causing weakness of the heart muscle (cardiomyopathy).OK, while our sages are thinking about heart issues:
I had 3 episodes of atrial flutter 5 years ago, cured by 2 x atrial reversions, 1 x extra dose of beta blocker. Only occasional bursts lasting seconds since then. None is past 6+ months; I'm not concerned.
I have a 'minor' blockage of one smaller heart artery ('minimal stenosis' CAD RAD score of 1). On stains and Xeralto as precautions.
But I've had issues with ectopic beats since then. Atrial and ventricular; can't say the proportions. I have a 6 channel 'Kardia' ECG device which I can send readings to my cardiologist if necessary or prior to a particular appointment.
I can get a lot of ectopics - every second beat over a few minutes, then various numbers on-and-off over hours; a couple of hours later, more. I call them 'swarms'. They bug me, especially when I am trying to sleep, with the 'thump' of the catch-up beat impossible to ignore.
I was on Sotalol beta blocker after the atrial flutter and increased dosages helped with the ectopics. Eventually they 'broke through' that; tried metoprolol but no help; back to Sotalol, then back they came - talking over a year or two so far here. Changed to amiodarone for about 2 months and that stopped the ectopics, at least the ones I noticed. Checked thyroid - OK. Came off the amiodarone (I know it not great to take) and the ectopics held off for about 3 months, then returned. Cardiologist disappointed. Back on Sotalol, stopped the ectopics again. But after several months, back they came.
So I'm back on amiodarone but it hasn't stopped them this time. Not the 'constant' runs but plenty, and often 'heavy'.
Cardiologist said a while back they they don't now of any particular causative agent for increased ectopics, although I see a positive correlation with being tired (in general, or after a particular bad night's sleep) and/or being hot.
SO: I'm not looking for any particular advice here about what to do, but I'm seeing my cardiologist in the new year and we'll be discussing situation. What are some things I can mention, ask about, explore with him? Other therapies? I've heard about an operation to 'cauterise' the extra beat-initiating locii within the heart - is that just for atrial flutter, or possible for ectopics?
And thank you every one for tuning in
AFF Supporters can remove this and all advertisements
The one you saw was not an atrial ectopic - that was a ventricular response to an atrial ectopic - which is how you felt it. You don't feel atrial ectopics unless there is a ventricular response (an extra heart beat = PVC)Not sure why you say a lot
Correct - EPS/RFA only offered if the ectopics are symptomatic and not controlled by the usual meds. Generally, single ectopics are not considered for EPS/RFA - it's mainly if you are getting runs of them (=sustained). Such a run of 3 consecutive PVC.) you can have an ablation for premature ventricular surgery contractions if they’re very frequent and highly symptomatic (>15% of total beats on Holter) or the PVCs are causing weakness of the heart muscle (cardiomyopathy).
What I'm seeing is a ECG that looks like atrial flutter.
The atrial rate at 150 is too slow for atrial flutter. The first wave you have marked looks like a U wave to me. It’s slightly different to the second wave. The second wave doesn’t appear in the lead 111 trace either so maybe not an atrial wave. Needs a proper ECG,Which is why I'm not saying it is - just looks like one. It may well be normal. Here is a real one
View attachment 355112
Here are what I think are atrial ectopics in lead II
View attachment 355113



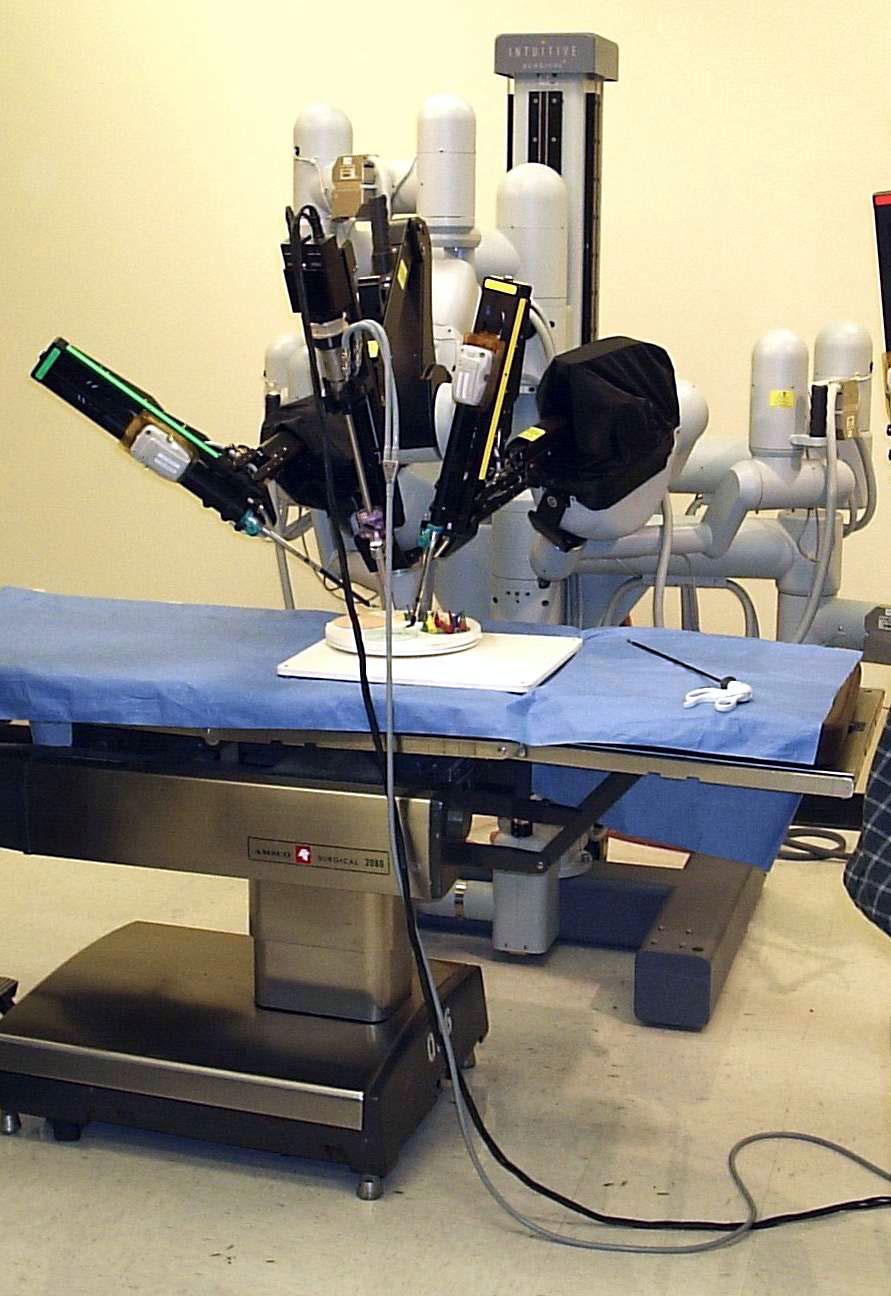
The Robot
One of the 4 arms will carry the camera module.
View attachment 355154
The surgeons controls
The big thing is the screen projector
All fly by wire (blue fibre optic)
Surgeon scrubs up for initial placement of the arms, scrubs up at the end for closing the holes. But in between with at the terminal - can be unscrubbed
Controls are feet pedals and articulating arms under the projector - to the left of the circular bit just above the black and white rail in the last photo
View attachment 355156View attachment 355155
Apart from prostatectomy, does the Da Vinci unit have other uses?

Many thanks @Steamrollersam . A few follow-ups, please.
* What do you mean by 'sustained' - as in number over a particular time (say, hours), or occurring and and off for years?
* You say PVCs are mapped using the software - not atrial ectopics?
* Is it ever done to have an electrophysiology study via catheter just to map, or they sometimes go in and then decide there are too many sites to ablate?
I hear what you are saying re an ablation being overkill. I don't know the proportions of PVCs Vs PAC; like I said, the ectopics took a holiday during my Holter study (I could tell - I wasn't feeling them).
I have a mate in Toronto who has suffered from afib for 20 years and has had 4 ablations since 2008 - the most recent a few weeks ago. In 2008, the procedure was new, so he went to Cleveland Clinic, where it was apparently perfected. His afib/flutter returns after a few years each time. Now routine in Ontario (as I would expect) and for him its like going to the dentist. But that's all for afib.
Thanks all for the input. I'll see what my cardiologist says; I trust him very much but its good to be armed with some concepts to explore, or at least know a bit about if they arise in discussion.
Sustained would be a few beats in a row, how many tends to be arbitrary. Premature atrial contractions (PACs) and premature ventricular contractions (PVCs) are just an extra beat every so often; they don’t happen in a row but they can be frequent which seems to be the case with you. It would be unusual for PACs to come just from one focus. In contrast PVCs in some people can just come from one spot in the heart (the outflow tract) and this is easily ablated; other foci may be on the surface of the heart or on the inside of the left ventricle—these are tricky to ablate and risky too.Many thanks @Steamrollersam . A few follow-ups, please.
* What do you mean by 'sustained' - as in number over a particular time (say, hours), or occurring and and off for years?
* You say PVCs are mapped using the software - not atrial ectopics?
* Is it ever done to have an electrophysiology study via catheter just to map, or they sometimes go in and then decide there are too many sites to ablate?
I hear what you are saying re an ablation being overkill. I don't know the proportions of PVCs Vs PAC; like I said, the ectopics took a holiday during my Holter study (I could tell - I wasn't feeling them).
I have a mate in Toronto who has suffered from afib for 20 years and has had 4 ablations since 2008 - the most recent a few weeks ago. In 2008, the procedure was new, so he went to Cleveland Clinic, where it was apparently perfected. His afib/flutter returns after a few years each time. Now routine in Ontario (as I would expect) and for him its like going to the dentist. But that's all for afib.
Thanks all for the input. I'll see what my cardiologist says; I trust him very much but it’s good to be armed with some concepts to explore, or at least know a bit about if they arise in discussion.
I get regular sharp pain going through left shoulder / collarbone. Feels electrical to me so would hazard a guess some sort of nerve pain associated with the tendonitis/bursitis that was diagnosed in the shoulder around 20 years ago.last weeks random pain in my shoulder, doctor suggested it was a muscle spasm of some sort, its cleared itself.

